Diabetic Retinopathy
Diabetic retinopathy, a common complication of diabetes mellitus, is a major cause of vision impairment and blindness among working-age adults. This condition arises from damage to the retinal blood vessels due to chronic hyperglycemia. The prevalence of diabetes is increasing globally, making diabetic retinopathy a growing public health concern. This paper aims to provide a comprehensive understanding of diabetic retinopathy, encompassing its pathophysiology, risk factors, symptoms, diagnostic methods, and treatment options. By enhancing our understanding of this condition, we can improve prevention, early detection, and management, thereby reducing the burden of vision loss.

Normal Retinal Function
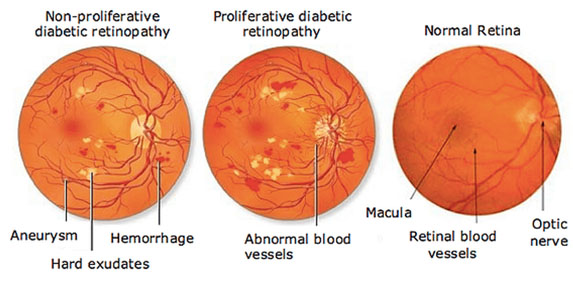
The retina is a layer of tissue at the back of the eye responsible for converting light into neural signals sent to the brain. It consists of photoreceptors, blood vessels, and supportive tissues that maintain visual function. In a healthy eye, light passes through the cornea and lens, focusing on the retina to form clear images.
Hyperglycemia and Retinal Damage
Chronic hyperglycemia is the primary factor leading to retinal damage in diabetic retinopathy. Elevated blood glucose levels cause biochemical changes in the retinal microvasculature, leading to a cascade of pathological events. The accumulation of advanced glycation end-products (AGEs) and increased oxidative stress damage endothelial cells and pericytes, disrupting the blood-retinal barrier.
- Microvascular Changes: Early changes include capillary basement membrane thickening, microaneurysms, and pericyte loss. These changes result in capillary leakage, retinal edema, and formation of hard exudates.
- Oxidative Stress and Inflammation: Hyperglycemia induces oxidative stress and inflammatory pathways, contributing to endothelial dysfunction and further vascular damage.
- Neovascularization: In response to retinal ischemia, hypoxia-inducible factors stimulate the production of vascular endothelial growth factor (VEGF), leading to the formation of fragile new blood vessels. These vessels are prone to bleeding, causing vitreous hemorrhage and tractional retinal detachment.
Stages of Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR): The early stage, characterized by microaneurysms, dot-and-blot hemorrhages, hard exudates, and retinal edema. NPDR can progress from mild to moderate and severe, depending on the extent of vascular abnormalities.
- Proliferative Diabetic Retinopathy (PDR): The advanced stage marked by neovascularization. New blood vessels form on the retinal surface and optic disc, which can lead to severe complications such as vitreous hemorrhage and tractional retinal detachment.
- Diabetic Macular Edema (DME): A condition where fluid accumulates in the macula, the central part of the retina responsible for detailed vision. DME can occur at any stage of diabetic retinopathy and is a leading cause of vision loss in diabetic patients.
Duration of Diabetes
The risk of developing diabetic retinopathy increases with the duration of diabetes. Studies show that nearly all patients with type 1 diabetes and more than 60% of those with type 2 diabetes develop some degree of retinopathy after 20 years of disease.
Glycemic Control
Poor glycemic control is strongly associated with the onset and progression of diabetic retinopathy. Maintaining optimal blood glucose levels reduces the risk of retinopathy and slows its progression. The Diabetes Control and Complications Trial (DCCT) and the UK Prospective Diabetes Study (UKPDS) demonstrated the benefits of tight glycemic control in reducing the incidence of retinopathy.
Hypertension
Hypertension exacerbates retinal vascular damage and increases the risk of diabetic retinopathy. Controlling blood pressure through lifestyle modifications and medications is crucial in managing the risk.
Dyslipidemia
Abnormal lipid levels contribute to the development of hard exudates and macular edema in diabetic retinopathy. Managing dyslipidemia with statins and other lipid-lowering agents can help reduce retinal complications.
Pregnancy
Pregnant women with pre-existing diabetes or gestational diabetes have an increased risk of developing or worsening diabetic retinopathy. Pregnancy accelerates the progression of retinopathy, necessitating close monitoring and management.
Genetic Factors
Genetic predispositions play a role in susceptibility to diabetic retinopathy. Research is ongoing to identify specific genetic markers associated with the condition.
Lifestyle Factors
Lifestyle choices such as smoking, physical inactivity, and poor diet can contribute to the development and progression of diabetic retinopathy. Encouraging healthy lifestyle habits is essential for reducing the risk.
Early Symptoms
In the early stages, diabetic retinopathy is often asymptomatic. Patients may not notice any changes in vision until the disease has progressed significantly. Early signs that may go unnoticed include microaneurysms and minor hemorrhages.
Progressive Symptoms
As diabetic retinopathy progresses, patients may experience:
- Blurred Vision: Difficulty seeing clearly, especially during activities like reading or driving.
- Floaters: Dark spots or strings floating in the field of vision due to vitreous hemorrhage.
- Dark or Empty Areas in Vision: Blind spots in the visual field caused by retinal ischemia.
- Difficulty Seeing at Night: Impaired night vision due to retinal damage.
Complications
Advanced diabetic retinopathy can lead to severe complications, including:
- Vitreous Hemorrhage: Bleeding into the vitreous humor, causing sudden vision loss.
- Tractional Retinal Detachment: The formation of scar tissue that pulls the retina away from its normal position.
- Neovascular Glaucoma: Increased intraocular pressure due to neovascularization obstructing the eye’s drainage system.
These complications can result in significant vision loss or blindness if left untreated.
Clinical Examination
Early detection of diabetic retinopathy relies on comprehensive eye examinations performed by optometrists or ophthalmologists. These examinations include:
- Dilated Fundus Examination: The use of an ophthalmoscope to examine the retina through a dilated pupil, allowing for a detailed view of retinal structures and identification of abnormalities.
- Fundus Photography: Imaging of the retina to document and monitor changes over time.
Diagnostic Tests
Advanced diagnostic tools enhance the detection and assessment of diabetic retinopathy:
- Fluorescein Angiography: A diagnostic test involving the injection of fluorescein dye into the bloodstream. The dye highlights the retinal blood vessels, allowing for the identification of leakage, microaneurysms, and neovascularization.
- Optical Coherence Tomography (OCT): A non-invasive imaging technique that provides high-resolution cross-sectional images of the retina. OCT is particularly useful for assessing retinal thickness and detecting diabetic macular edema.
- OCT Angiography (OCTA): A newer technology that visualizes blood flow in the retina without the need for dye injection. OCTA helps identify areas of non-perfusion and neovascularization.
These diagnostic methods are crucial for accurately diagnosing the stage of diabetic retinopathy and guiding treatment decisions.
Preventive Strategies
Preventive measures are vital in managing diabetic retinopathy:
- Glycemic Control: Maintaining optimal blood glucose levels is the cornerstone of preventing and managing diabetic retinopathy. Regular monitoring of blood sugar levels, adherence to diabetes medications, and lifestyle modifications are essential.
- Blood Pressure Management: Controlling hypertension through medications and lifestyle changes reduces the risk of retinal damage.
- Lipid Management: Using statins and other lipid-lowering agents to manage dyslipidemia can help prevent retinal complications.
- Regular Eye Examinations: Routine eye exams are crucial for early detection and intervention. Patients with diabetes should have annual dilated eye exams.
Medical Treatments
Several medical treatments are available to manage diabetic retinopathy:
- Anti-VEGF Therapy: Intravitreal injections of anti-VEGF agents (e.g., ranibizumab, aflibercept) inhibit the growth of abnormal blood vessels and reduce macular edema. These injections are effective in treating both proliferative diabetic retinopathy and diabetic macular edema.
- Corticosteroids: Intravitreal corticosteroid injections reduce inflammation and macular edema. They are an option for patients who do not respond to anti-VEGF therapy.
Laser Therapy
Laser therapy is a well-established treatment for diabetic retinopathy:
- Focal/Grid Laser Photocoagulation: This technique targets specific areas of leakage in diabetic macular edema to reduce fluid accumulation and stabilize vision.
- Panretinal Photocoagulation (PRP): PRP is used to treat proliferative diabetic retinopathy. The laser creates controlled burns in the peripheral retina to reduce neovascularization and prevent complications.
Surgical Interventions
In advanced cases, surgical interventions may be necessary:
- Vitrectomy: A surgical procedure to remove vitreous hemorrhage or scar tissue causing tractional retinal detachment. Vitrectomy can restore vision and prevent further damage.
- Retinal Detachment Surgery: Procedures to repair retinal detachment, which may involve scleral buckling, vitrectomy, or pneumatic retinopexy.
These treatments are tailored to the individual patient’s condition and aim to preserve or restore vision.
Patient Education
Educating patients about the risks of diabetic retinopathy and the importance of regular monitoring is crucial. Patients should understand the impact of diabetes on their eyes and the need for strict glycemic control and routine eye exams.
Lifestyle Modifications
Encouraging healthy lifestyle habits can significantly reduce the risk of diabetic retinopathy:
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins helps maintain blood sugar levels.
- Regular Exercise: Physical activity improves insulin sensitivity and helps control blood glucose levels.
- Smoking Cessation: Smoking cessation reduces the risk of vascular damage and progression of diabetic retinopathy.
Prognosis
With proper management, the prognosis for patients with diabetic retinopathy can be favorable. Early detection and intervention are key to preventing vision loss. Anti-VEGF therapy, laser treatments, and surgical interventions have significantly improved outcomes for patients. However, continued vigilance and adherence to treatment protocols are essential to maintaining vision and preventing complications.
Diabetic retinopathy is a major complication of diabetes that requires comprehensive management to prevent vision loss. Early detection through regular eye exams, tight glycemic control, and prompt treatment are essential. Ongoing research and advances in medical technology hold promise for better management and outcomes for patients with diabetic retinopathy. By understanding the pathophysiology, risk factors, and treatment options, healthcare providers can improve patient care and reduce the burden of this vision-threatening condition.
References:
Boyd, K. (2019, October 24). What Is Diabetic Retinopathy? American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
Diabetic Eye Conditions – Hesed Eye Specialists Singapore. (n.d.). Https://Eyedoc.sg/. https://eyedoc.sg/diabetic-eye-conditions/