Pediatric Ophthalmology
Pediatric ophthalmology is a specialized branch of medicine dedicated to diagnosing and treating eye disorders in children, ranging from newborns to adolescents. The development of the visual system is a complex and dynamic process that starts before birth and continues throughout childhood. Early detection and timely treatment of pediatric eye conditions are essential to prevent permanent visual impairment, which can significantly impact a child’s learning, development, and quality of life.
This guide provides an in-depth look at the critical aspects of pediatric ophthalmology, including the development of the visual system, common eye conditions in children, diagnostic techniques, surgical interventions, and special considerations for different pediatric populations. Additionally, we will explore current trends and future directions in this field, providing a foundation for further study or clinical practice.

Development of the Visual System in Children
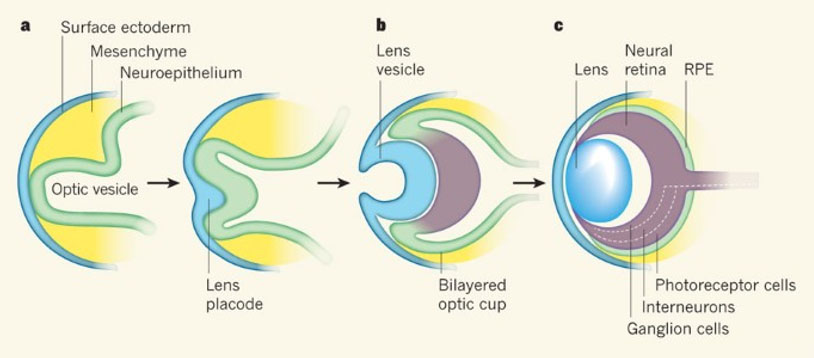
The development of the human eye begins early in embryogenesis, around the third week of gestation. The eye originates from three primary tissues: the neuroectoderm, surface ectoderm, and mesoderm. The optic vesicles, derived from the neuroectoderm, evaginate from the diencephalon to form the optic cups, which eventually give rise to the retina, optic nerve, and other neural components of the eye. The surface ectoderm forms the lens and corneal epithelium, while the mesoderm contributes to the vascular and connective tissues, including the choroid, sclera, and extraocular muscles.
By the seventh week of gestation, the rudimentary structures of the eye, including the cornea, lens, and retina, are established. The fetal period involves the differentiation and maturation of these structures. For example, retinal photoreceptors begin to develop around the 20th week of gestation, and the central visual pathways continue to mature postnatally. Proper embryonic development is crucial, as disruptions can lead to congenital anomalies such as anophthalmia, microphthalmia, or coloboma.
Postnatal Development of the Visual System
After birth, the visual system continues to develop, with significant milestones occurring during the first few years of life. At birth, the visual acuity of a newborn is approximately 20/400, with limited color vision and contrast sensitivity. The development of visual acuity is closely linked to the maturation of the fovea and the refinement of neural connections in the visual cortex.
During the first six months, visual acuity rapidly improves, reaching approximately 20/25 by the age of two years. Binocular vision, or the ability to use both eyes together, develops during this period, facilitating depth perception. Eye alignment and coordination also improve, allowing for smoother and more precise eye movements.
Milestones in Visual Development
Several visual milestones can be observed in infants and young children:
- 0-3 months: Eye contact, fixation on faces, and tracking moving objects.
- 4-6 months: Improved focus, recognition of familiar faces, and beginning of hand-eye coordination.
- 7-12 months: Better depth perception, reaching for objects, and more refined eye-hand coordination.
- 1-2 years: Development of fine visual skills, such as recognizing shapes, colors, and objects at a distance.
Common Developmental Disorders
Disruptions in the normal development of the visual system can lead to a range of disorders. Amblyopia, commonly known as “lazy eye,” occurs when the brain favors one eye over the other, leading to reduced vision in the affected eye. Strabismus, or misalignment of the eyes, can also interfere with binocular vision and depth perception. Early identification and treatment of these conditions are vital to prevent long-term visual impairment.
Refractive Errors
Refractive errors occur when the eye does not focus light correctly on the retina, resulting in blurred vision. In children, the most common refractive errors include myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
- Myopia: This condition is characterized by the eye being too long, causing light to focus in front of the retina. Myopic children may have difficulty seeing distant objects clearly.
- Hyperopia: In hyperopia, the eye is too short, resulting in light focusing behind the retina. Children with hyperopia may have difficulty focusing on close objects, although mild hyperopia is common and often does not require correction.
- Astigmatism: This occurs when the cornea is irregularly shaped, causing light to focus unevenly on the retina. Astigmatism can result in distorted or blurred vision at all distances.
Diagnosis and Management Refractive errors are diagnosed through a comprehensive eye examination, including retinoscopy and refraction tests. Corrective lenses, such as glasses or contact lenses, are the primary treatment for refractive errors in children. Regular follow-up is essential to monitor changes in vision and adjust prescriptions as needed.
Amblyopia
Amblyopia, commonly referred to as “lazy eye,” is a condition where one eye has reduced vision that cannot be corrected solely by glasses or contact lenses. It occurs when the brain favors one eye over the other, leading to poor visual development in the affected eye.
Etiology and Types Amblyopia can arise from several causes:
- Strabismic Amblyopia: Caused by strabismus, where the misalignment of the eyes prevents proper binocular vision.
- Refractive Amblyopia: Results from significant refractive errors in one eye that are not corrected early.
- Deprivation Amblyopia: Occurs when an obstruction, such as a congenital cataract, prevents visual input from reaching the retina.
Clinical Presentation Children with amblyopia may not have noticeable symptoms, making it crucial to screen for the condition during routine eye exams. Signs may include poor depth perception, eye strain, or a tendency to favor one eye over the other.
Treatment and Prognosis Treatment involves forcing the brain to use the weaker eye, typically through patching the stronger eye or using atropine drops to blur vision in the stronger eye. Early detection and treatment are critical, as the prognosis for amblyopia is significantly better when intervention occurs before the age of seven.
Strabismus
Strabismus is a condition where the eyes are misaligned and do not move together. It can be present at birth or develop later in childhood.
Types of Strabismus
- Esotropia: Inward turning of the eye.
- Exotropia: Outward turning of the eye.
- Hypertropia: Upward turning of the eye.
- Hypotropia: Downward turning of the eye.
Diagnostic Approach The diagnosis of strabismus involves a thorough eye examination, including visual acuity testing, cover tests, and assessment of ocular motility. Identifying the underlying cause is essential for determining the appropriate treatment.
Treatment Options Treatment for strabismus may include corrective glasses, prism lenses, vision therapy, or surgical correction. The goal is to improve eye alignment and binocular vision.
Congenital Cataracts
Congenital cataracts are opacities in the lens of the eye present at birth or developing shortly thereafter. They can lead to significant visual impairment if not treated promptly.
Causes and Diagnosis Congenital cataracts can result from genetic mutations, intrauterine infections, metabolic disorders, or idiopathic causes. Diagnosis typically involves a red reflex test and further evaluation with slit-lamp examination and imaging as needed.
Management Early surgical removal of the cataract is usually necessary to prevent amblyopia and promote normal visual development. Postoperative care may include the use of corrective lenses or contact lenses and regular follow-up to monitor visual progress.
Retinopathy of Prematurity (ROP)
ROP is a disorder of the developing retinal blood vessels that occurs in premature infants. It can lead to retinal detachment and blindness if not treated.
Risk Factors and Stages Risk factors for ROP include low birth weight, early gestational age, and oxygen therapy. The condition is classified into five stages, with Stage 1 being mild and Stage 5 indicating total retinal detachment.
Screening and Treatment Routine screening for ROP is recommended for premature infants. Treatment options include laser therapy, cryotherapy, or intravitreal injections to halt the progression of abnormal blood vessel growth.
Visual Acuity Testing
Visual acuity testing in children requires age-appropriate methods to ensure accurate assessment. In infants and young children, preferential looking techniques, such as the Teller Acuity Cards, are used to estimate visual acuity. Older children can be tested using symbol-based charts like the LEA symbols or HOTV chart.
Interpretation of Results Understanding normal visual acuity milestones for different age groups is essential for interpreting test results. Any deviation from these norms may indicate an underlying visual disorder that requires further investigation.
Ocular Alignment and Motility Testing
Proper ocular alignment and motility are crucial for binocular vision. Several tests are used to assess these aspects in pediatric patients:
- Cover Test: This test identifies misalignment by covering one eye while observing the movement of the uncovered eye.
- Hirschberg Test: This test estimates the degree of strabismus by observing the reflection of light on the corneas.
Assessment of Eye Movements Evaluating the full range of eye movements is essential to identify any limitations or abnormal patterns that could indicate underlying conditions, such as cranial nerve palsies or muscular disorders.
Fundus Examination
A thorough fundus examination is essential for detecting retinal and optic nerve abnormalities in children. In young patients, the examination may require the use of a binocular indirect ophthalmoscope, often with the aid of pharmacologic dilation to provide a better view of the posterior segment.
Identification of Common Abnormalities Fundus examination can reveal a variety of conditions, including retinoblastoma, retinal detachment, and optic nerve anomalies. Early detection of these conditions is crucial for preventing vision loss.
Imaging and Other Diagnostic Tools
Advanced imaging techniques and diagnostic tools are increasingly being used in pediatric ophthalmology:
- Ultrasound: Useful for evaluating the eye when the view is obscured by media opacities, such as cataracts.
- Optical Coherence Tomography (OCT): Provides detailed images of retinal layers, helping diagnose conditions like macular edema and optic nerve abnormalities.
- Electroretinography (ERG): Assesses retinal function, particularly in conditions like retinitis pigmentosa and congenital stationary night blindness.
Indications for Surgery
Surgical intervention in pediatric ophthalmology is often indicated when conservative treatments are ineffective, or when there is a risk of permanent visual impairment. Conditions that may require surgery include strabismus, congenital cataracts, and advanced stages of retinopathy of prematurity (ROP).
Common Pediatric Ophthalmic Surgeries
- Strabismus Surgery: Involves adjusting the position of the extraocular muscles to improve eye alignment. Early surgery can prevent the development of amblyopia and improve binocular vision.
- Cataract Extraction: Surgery to remove congenital cataracts is typically performed within the first few weeks of life to prevent deprivation amblyopia. The procedure may be followed by the implantation of an intraocular lens or the use of contact lenses.
- ROP Laser Treatment: Laser photocoagulation is used to ablate avascular retinal tissue in infants with severe ROP, reducing the risk of retinal detachment.
Preoperative and Postoperative Care
Special considerations are required for pediatric patients undergoing eye surgery:
- Preoperative Care: This includes a thorough examination to assess the child’s overall health and any anesthetic risks. Parents should be counseled on the procedure, risks, and expected outcomes.
- Postoperative Care: Close monitoring is essential to detect complications such as infection, glaucoma, or retinal detachment. Regular follow-up visits are necessary to ensure proper healing and visual development.
Children with Systemic Diseases
Certain systemic conditions can have significant ocular manifestations:
- Down Syndrome: Children with Down syndrome are at increased risk for conditions like cataracts, strabismus, and refractive errors.
- Diabetes: Pediatric diabetes can lead to diabetic retinopathy, although this is less common in younger children. Regular screening is essential for early detection.
- Juvenile Idiopathic Arthritis (JIA): JIA can cause uveitis, leading to vision-threatening complications if not managed appropriately.
Children with Developmental Delays
Children with developmental delays may present unique challenges in ophthalmologic evaluation and treatment. These children are at higher risk for refractive errors, strabismus, and amblyopia. Tailored approaches, including more frequent screenings and collaboration with other healthcare providers, are necessary to ensure optimal outcomes.
Pediatric Ocular Trauma
Ocular trauma is a significant cause of visual impairment in children. Common causes include sports injuries, accidents, and foreign bodies. Prompt assessment and treatment are critical to prevent long-term damage.
Prevention and Management
- Prevention: Education on eye safety, particularly in sports and at home, is crucial for preventing injuries.
- Management: Treatment may range from conservative management for minor injuries to surgical intervention for more severe trauma, such as globe rupture or retinal detachment.
Advances in Genetic Therapies
The field of pediatric ophthalmology is poised for significant advancements with the development of genetic therapies. Conditions like Leber’s congenital amaurosis (LCA) and retinitis pigmentosa, once considered untreatable, are now the focus of gene therapy research. The introduction of treatments like Luxturna, the first FDA-approved gene therapy for a retinal disorder, marks the beginning of a new era in pediatric ophthalmology.
Innovations in Diagnostic Tools
The integration of artificial intelligence (AI) and machine learning into diagnostic tools is revolutionizing the early detection of pediatric eye diseases. AI algorithms can analyze retinal images for signs of disease, improving diagnostic accuracy and allowing for earlier intervention.
Emerging Treatments
Research is ongoing into new pharmacologic treatments for conditions such as amblyopia, where drug therapies may complement or replace traditional methods like patching. Additionally, advances in minimally invasive surgical techniques are improving outcomes and reducing recovery times for pediatric patients.
Pediatric ophthalmology is a vital field that requires a deep understanding of the unique challenges and conditions affecting the visual system in children. From the early development of the eye to the management of complex disorders, this guide provides a comprehensive overview for medical students looking to deepen their knowledge in this area. Early diagnosis and intervention are crucial in pediatric ophthalmology, making continuous learning and research essential for improving outcomes and advancing the field. As technology and treatments evolve, the future of pediatric eye care looks promising, offering new hope for young patients with visual impairments.
References:
Wright, K. W., Strube, Y. N., & Thompson, L. S. (2012). Pediatric ophthalmology and strabismus (3rd ed.). Oxford University Press. https://doi.org/10.1093/med/9780199857012.001.0001
Lambert, S. R., & Lyons, C. J. (Eds.). (2017). Taylor and Hoyt’s pediatric ophthalmology and strabismus (5th ed.). Elsevier. https://doi.org/10.1016/B978-0-7020-6197-1.00001-9
Repka, M. X., & Lum, F. (2011). Pediatric eye disease investigator group: 15-year update on major studies. Journal of the American Association for Pediatric Ophthalmology and Strabismus, 15(5), 457-463. https://doi.org/10.1016/j.jaapos.2011.07.017