Strabismus
Strabismus, commonly known as “crossed eyes,” is a condition in which the eyes do not properly align with each other when looking at an object. This misalignment can occur in various directions: one eye may turn inward, outward, upward, or downward while the other eye focuses on an object. Strabismus can be constant or intermittent and can affect one or both eyes.

Normally both eyes aim at the same spot and the brain combines both images from both eyes into a single 3D image, this is how we can tell if something is near or far and this is called depth perception. When the eyes are not aligned during childhood the brain ignores the image from the misaligned eye and only the image from the straight eye is processed by the brain. In this case depth perception is affected.
If the eyes are properly oriented during childhood, vision should develop well. But if the eyes are not aligned, a condition called amblyopia, also known as lazy eye, can develop. This is the phenomenon when the poorly focused eye has poor vision.
Strabismus in children can be caused by various factors, often related to the development and coordination of the eyes. The most common cause is if the child is nearsighted or farsighted because if they have blurry vision the eyes strain to see clearly. This straining causes the child’s eye to cross or drift apart, but when they wear glasses their eye alignment can improve as well. Other causes include:
- Genetic predisposition and a family history of strabismus
- Premature birth
- Neurological disorders
- Hydrocephalus
- Brain tumor
- Cataracts
- Down syndrome
- Cataracts
- Eye injury
Most children don’t have any of these problems and develop strabismus without an obvious cause.
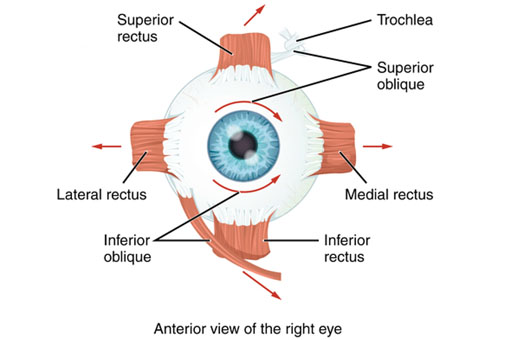
There are six extraocular muscles that control eye movements. Below is a brief summary of the muscles function and their innervation:
- Medial Rectus:
- Function: Moves the eye inward, towards the nose (adduction).
- Nerve Supply: Oculomotor nerve (Cranial Nerve III).
- Lateral Rectus:
- Function: Moves the eye outward, away from the nose (abduction).
- Nerve Supply: Abducens nerve (Cranial Nerve VI).
- Superior Rectus:
- Function: Moves the eye upward (elevation) and slightly inward (intorsion and adduction).
- Nerve Supply: Oculomotor nerve (Cranial Nerve III).
- Inferior Rectus:
- Function: Moves the eye downward (depression) and slightly inward (extorsion and adduction).
- Nerve Supply: Oculomotor nerve (Cranial Nerve III).
- Superior Oblique:
- Function: Moves the eye downward (depression) and outward (abduction and intorsion).
- Nerve Supply: Trochlear nerve (Cranial Nerve IV).
- Inferior Oblique:
- Function: Moves the eye upward (elevation) and outward (abduction and extorsion).
- Nerve Supply: Oculomotor nerve (Cranial Nerve III).
Functional Summary
- Horizontal Movements:
- Adduction: Medial rectus.
- Abduction: Lateral rectus.
- Vertical Movements:
- Elevation: Superior rectus (also intorts and adducts), Inferior oblique (also extorts and abducts).
- Depression: Inferior rectus (also extorts and adducts), Superior oblique (also intorts and abducts).
- Torsional Movements:
- Intorsion: Superior oblique, Superior rectus.
- Extorsion: Inferior oblique, Inferior rectus.
Understanding the functions of these muscles is essential in diagnosing and treating conditions related to eye movement disorders, such as strabismus and cranial nerve palsies.
Overactive or Underactive Muscles: When one or more muscles are stronger or weaker than they should be, the eyes can become misaligned. For example, if the medial rectus muscle is too strong compared to the lateral rectus muscle, the eye may turn inward, causing esotropia.
Nerve Dysfunction: The cranial nerves (III, IV, and VI) that innervate these muscles may be damaged or not functioning correctly, leading to improper muscle control.
- Cranial Nerve III (Oculomotor): Controls the medial rectus, superior rectus, inferior rectus, and inferior oblique muscles.
- Cranial Nerve IV (Trochlear): Controls the superior oblique muscle.
- Cranial Nerve VI (Abducens): Controls the lateral rectus muscle.
Signs of strabismus:
The signs and symptoms vary depending on the severity of the case.
- Child is looking in different directions at the same time.
- Double vision (diplopia)
- Squinting or closing one eye when focusing on an object
- Poor depth perception
- Eye strain: especially after focusing on an object
- Wandering eye: drifting eye especially when tired or stressed
Amblyopia (lazy eye)
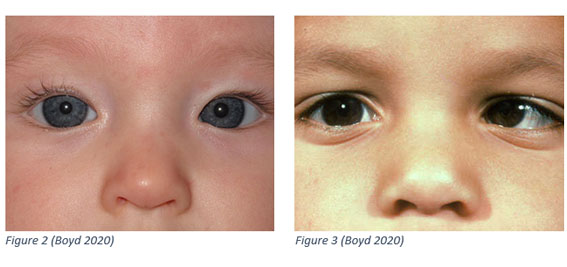
This is when a child less than one year old looks like he has crossed eyes when he doesn’t. this usually happens when a child has a wide flat nose and inner eyelid skin folds. The child usually outgrows pseudo strabismus.
Figure 1 is a photograph shows Pseudo strabismus, although they seem misaligned the light reflection is in the same place on both eyes. Figure 2 is a photograph shows off center light reflection on the left eye and this indicates strabismus.
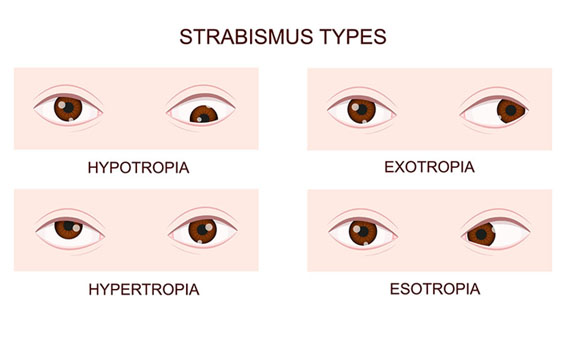
- Esotropia: Inward turning of the eye, often due to overactivity of the medial rectus muscle or underactivity of the lateral rectus muscle.
- Exotropia: Outward turning of the eye, often due to overactivity of the lateral rectus muscle or underactivity of the medial rectus muscle.
- Hypertropia: Upward turning of the eye, often due to overactivity of the superior rectus or inferior oblique muscle, or underactivity of the inferior rectus or superior oblique muscle.
- Hypotropia: Downward turning of the eye, often due to overactivity of the inferior rectus or superior oblique muscle, or underactivity of the superior rectus or inferior oblique muscle.
Other types of strabismus
- Infantile esotropia: Present from birth or develops within the first six months of life. The eyes turn inward significantly and consistently.
- Accommodative Esotropia: Typically develops between ages 2 and 4. It is associated with farsightedness (hyperopia) and occurs when the child focuses on nearby objects, causing the eyes to turn inward.
- Intermittent Exotropia: The eyes drift outward occasionally, especially when the child is tired, ill, or focusing on distant objects. It is the most common form of exotropia.
- Constant Exotropia: The eye consistently turns outward. This form is less common and may require more intensive treatment.
A complete eye exam and several testing methods are used to determine severity of the condition and develop an effective treatment plan. These include:
- Visual acuity
- Refraction
- Ocular alignment and movement test
- Cover test
- Hirschberg test (corneal light reflex test)
- Prism cover test
Glasses
When strabismus is due to eye strain because of blurry vision due to nearsightedness or farsightedness, or astigmatism, glasses help to align the eyes especially in cases of accommodative esotropia.
Prism lenses:
These lenses bend light entering the eye, helping to reduce the amount of eye turning needed to focus on an object and can alleviate double vision.
Vision therapy:
- Orthoptic exercises: A series of eye exercises designed to improve the coordination and focusing of the eyes.
- Computerized programs: These may include specific software designed to enhance binocular vision and eye coordination.
Patching:
- Covering the stronger eye: This forces the weaker eye to work harder, helping to improve its function and alignment. This is particularly useful in treating amblyopia (lazy eye) associated with strabismus.
Pharmacological Treatment:
- Atropine drops: Used in the stronger eye to blur vision temporarily, forcing the weaker eye to work harder, similar to patching.
- Botulinum toxin (Botox) injections: Injections into the eye muscles can temporarily weaken overactive muscles, helping to realign the eyes.
Strabismus surgery:
Involves adjusting the length or position of the eye muscles to improve alignment. This is typically considered when other treatments are not effective.
- Recession: Weakening an overactive muscle by reattaching it further back on the eye.
- Resection: Strengthening a weak muscle by cutting a portion and reattaching it.
- Plication: strengthening a weak muscle by folding it instead of cutting and reattaching.
- Transposition: moving the muscle to different position to correct vertical misalignment.
Click here to read more about strabismus surgery (add link)
- Regular monitoring: Frequent check-ups are essential to track progress and make any necessary adjustments to the treatment plan.
- Continued therapy: In some cases, ongoing vision therapy or use of prism lenses may be needed to maintain alignment and coordination.
Early and appropriate treatment of strabismus is crucial, especially in children, to ensure proper visual development and to prevent complications like amblyopia. For adults, treatment focuses on improving eye alignment and reducing symptoms like double vision.