Keratoplasty
Keratoplasty, or corneal transplantation, has revolutionized the treatment of various corneal diseases and injuries. It is one of the most successful types of transplantation performed today, with high rates of success and patient satisfaction. This paper delves into the different types of keratoplasty, their indications, and the latest advancements in surgical techniques.
Anatomy and Function of the Cornea
The cornea is a transparent, dome-shaped surface that covers the front of the eye. It plays a crucial role in focusing light onto the retina and protecting the eye from pathogens and injury. The cornea consists of five layers: the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and the endothelium. Damage to any of these layers can impair vision and necessitate keratoplasty.
Keratoplasty is indicated for various corneal conditions, including:
- Keratoconus: A progressive thinning of the cornea causing it to bulge into a cone shape.
- Fuchs’ Endothelial Dystrophy: A genetic disorder leading to the gradual loss of endothelial cells.
- Corneal Scarring: Due to infections, injuries, or previous surgeries.
- Bullous Keratopathy: Swelling of the cornea caused by endothelial dysfunction.
- Corneal Ulcers: Persistent, non-healing ulcers that threaten vision.
- Herpetic Keratitis: Severe infection of the cornea caused by herpes simplex virus.
There are several types of keratoplasty, each suited for different corneal conditions:
Penetrating Keratoplasty (PK)
PK involves replacing the full thickness of the cornea with a donor graft. It is commonly used for extensive corneal damage involving multiple layers.
Deep Anterior Lamellar Keratoplasty (DALK)
DALK selectively replaces the anterior layers of the cornea, preserving the patient’s healthy endothelium. It is ideal for conditions like keratoconus and stromal scars.
Descemet’s Stripping Endothelial Keratoplasty (DSEK)
DSEK involves the replacement of the endothelium and Descemet’s membrane while preserving the anterior corneal layers. It is commonly used for endothelial disorders like Fuchs’ dystrophy.
Descemet’s Membrane Endothelial Keratoplasty (DMEK)
DMEK is a refined version of DSEK, replacing only the Descemet’s membrane and endothelium. It offers faster visual recovery and fewer complications.
Keratoprosthesis
A keratoprosthesis, or artificial cornea, is used in patients with multiple graft failures or severe ocular surface diseases where donor tissue is unlikely to succeed.
The surgical approach varies depending on the type of keratoplasty:
Preoperative Preparation
- Evaluation: Detailed ocular examination, imaging, and patient history.
- Donor Tissue: Sourced from eye banks, evaluated for quality, and suitability.
- Anesthesia: Local or general anesthesia based on patient condition and surgeon preference.
Penetrating Keratoplasty (PK) Procedure
- Trephination: Removal of the diseased cornea using a trephine.
- Donor Graft: Preparation and sizing of the donor cornea.
- Suturing: Placement of the donor graft and securing with interrupted or continuous sutures.
DALK Procedure
- Stromal Dissection: Removal of the anterior stroma while preserving the endothelium.
- Air Injection: Creation of a plane between the stroma and Descemet’s membrane.
- Graft Placement: Securing the donor stroma with sutures.
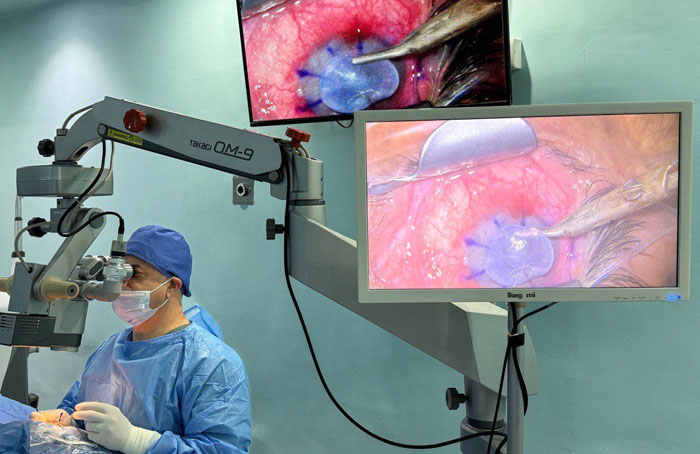
DSEK and DMEK Procedures
- Descemetorhexis: Removal of the patient’s Descemet’s membrane and endothelium.
- Graft Insertion: Folding and insertion of the donor tissue through a small incision.
- Unfolding and Positioning: Unfolding the graft and positioning it against the stroma using an air bubble.
- Medications: Topical antibiotics, steroids, and immunosuppressants.
- Follow-Up: Regular monitoring for graft clarity, rejection, and complications.
- Rehabilitation: Visual rehabilitation and management of astigmatism.
Outcomes and Success Rates
The success of keratoplasty depends on several factors, including the type of procedure, underlying condition, and patient compliance. Generally, keratoplasty boasts high success rates, with DMEK and DSEK showing rapid visual recovery and fewer complications compared to PK.
Complications
Potential complications include:
- Graft Rejection: Immune response against the donor tissue.
- Infection: Postoperative infections can jeopardize the graft.
- Glaucoma: Increased intraocular pressure following surgery.
- Astigmatism: Irregular corneal surface requiring correction.
- Primary Graft Failure: Failure of the graft to function immediately post-surgery.
Keratoplasty remains a cornerstone in the treatment of severe corneal diseases, offering the potential to restore vision and improve the quality of life for patients. Continued advancements in surgical techniques and postoperative care are essential to further enhance the success rates and reduce complications. Ophthalmology clinic professionals play a crucial role in patient education, preoperative preparation, and postoperative management to ensure optimal outcomes.