Keratoconus Management
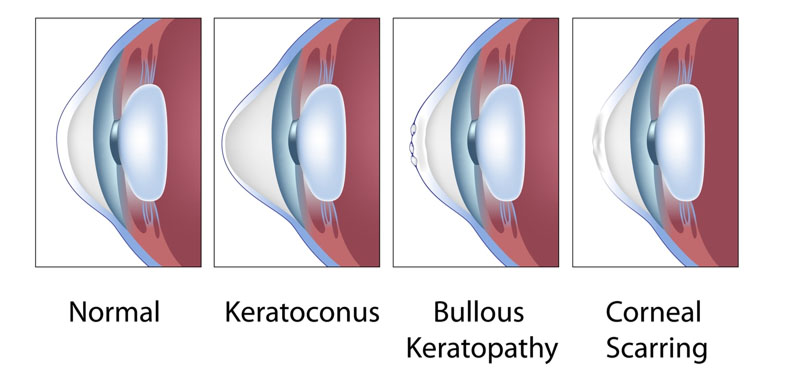
Keratoconus is a progressive eye disease in which the cornea, which is normally round, thins and begins to bulge into a cone-like shape. This cone shape deflects light as it enters the eye on its way to the retina, causing distorted vision. The exact cause of keratoconus is unknown, but it is thought to be related to a combination of genetic, environmental, and hormonal factors. Other associated causes are eye allergies, excessive eye rubbing, connective tissue disorders like eye allergies, excessive eye rubbing and connective tissue disorders such as Marfan syndrome and Ehlers Danlos syndrome.

Keratoconus is a progressive, degenerative disorder characterized by thinning and cone-like protrusion of the cornea. This condition typically begins in adolescence and can progress over a period of 10 to 20 years. As the cornea thins and bulges outward, it causes irregular astigmatism and myopia, leading to distorted and blurred vision.
Key features of keratoconus include:
- Corneal Thinning: The central or paracentral cornea becomes progressively thinner.
- Conical Protrusion: The cornea takes on a cone-like shape.
- Irregular Astigmatism: The uneven shape of the cornea leads to multiple focal points, causing distorted vision.
- Scarring: Advanced stages may involve scarring, which further impairs vision.
Corneal Ectasia is a condition that is similar to keratoconus but is typically induced by refractive surgery such as LASIK or PRK. The surgery weakens the corneal structure, leading to thinning and bulging similar to keratoconus. Ectasia can occur months or even years after the initial surgery, posing a challenge for both patients and clinicians.
Common characteristics of corneal ectasia include:
- Post-Surgical Onset: Often develops after refractive surgery.
- Progressive Thinning and Bulging: Similar to keratoconus, the cornea becomes thin and protrudes outward.
- Visual Distortion: Patients experience decreased visual acuity and quality of vision.
Understanding the anatomy and physiology of the cornea, as well as the pathophysiology of keratoconus and corneal ectasia, is crucial for comprehending the underlying principles and the need for treatments like corneal ring surgery. The irregularities in corneal shape and thickness disrupt normal vision, necessitating interventions that can restore corneal integrity and improve visual outcomes.
Early Stage
- Mild Corneal Thinning: The cornea begins to thin, but the changes are subtle and might not cause significant visual impairment.
- Slight Vision Changes: Patients may experience mild blurring or distortion of vision that can be corrected with eyeglasses or soft contact lenses.
- Initial Diagnosis: Keratoconus is often diagnosed during a routine eye exam or following complaints of visual changes.
Intermediate Stage
- Increased Corneal Thinning and Bulging: The corneal thinning becomes more pronounced, and the cornea starts to bulge more noticeably into a cone shape.
- More Pronounced Vision Distortion: Vision becomes more distorted and cannot be fully corrected with eyeglasses. Patients often need rigid gas permeable (RGP) contact lenses to achieve better vision.
- Irregular Astigmatism: Astigmatism caused by the irregular shape of the cornea becomes more severe.
Advanced Stage
- Severe Corneal Thinning and Steepening: The cornea becomes extremely thin and steepens significantly, leading to severe visual distortion.
- Scarring: Corneal scarring may occur, further impairing vision. This scarring often results from persistent eye rubbing or the progression of the disease itself.
- Hydrops: In rare cases, advanced keratoconus can lead to a condition called corneal hydrops, where fluid from inside the eye penetrates the cornea, causing sudden and painful swelling and a significant decrease in vision.
Diagnosing keratoconus typically involves a combination of a comprehensive eye exam and specialized tests to assess the shape and integrity of the cornea. Early detection is crucial as it allows for timely intervention, which can slow the progression of the disease and preserve vision. If keratoconus is suspected, an eye care professional may recommend more frequent examinations to closely monitor changes in the cornea.
Here are the key diagnostic methods:
Comprehensive Eye Exam
- Visual Acuity Test: Measures how well you can see at various distances.
- Refraction: Determines the prescription needed for corrective lenses.
Specialized Tests
- Corneal Topography:
- Description: This is the most important test for diagnosing keratoconus. It creates a detailed map of the curvature of the cornea.
- Purpose: Detects irregularities in the corneal shape that are characteristic of keratoconus.
- Pachymetry:
- Description: Measures the thickness of the cornea using ultrasound or optical methods.
- Purpose: Helps to detect thinning of the cornea, a hallmark of keratoconus.
The treatment of keratoconus varies depending on the stage of the disease and the severity of symptoms. The goal of treatment is to stabilize the cornea, improve vision, and prevent further progression of the disease. Here are the main treatment options:
Early Stage Treatment
- Eyeglasses and Soft Contact Lenses:
- For mild cases, vision can often be corrected with eyeglasses or soft contact lenses.
- Corneal Cross-Linking (CXL):
- Purpose: To strengthen the corneal tissue and halt the progression of keratoconus.
- Procedure: Riboflavin (vitamin B2) eye drops are applied to the cornea, which is then exposed to ultraviolet (UV) light. This causes the collagen fibers in the cornea to cross-link, strengthening the cornea.
- Eyeglasses and Soft Contact Lenses:
Intermediate Stage Treatment
- Rigid Gas Permeable (RGP) Contact Lenses:
- These lenses provide a smooth surface over the irregular cornea, improving vision.
- Scleral and Hybrid Lenses:
- Scleral Lenses: Larger lenses that vault over the cornea and rest on the sclera (white part of the eye), providing a smooth optical surface.
- Hybrid Lenses: Combine a hard central lens with a soft outer ring for comfort and better vision correction.
- Intacs (Intracorneal Ring Segments):
- Purpose: To flatten the cornea and improve vision.
- Procedure: Small, crescent-shaped plastic inserts are placed within the cornea to alter its shape.
- Rigid Gas Permeable (RGP) Contact Lenses:
Advanced Stage Treatment
- Corneal Transplantation (Keratoplasty):
- Types: Penetrating keratoplasty (full-thickness transplant) or deep anterior lamellar keratoplasty (DALK, partial-thickness transplant).
- Purpose: To replace the diseased cornea with a healthy donor cornea in cases where other treatments are ineffective.
- Corneal Transplantation (Keratoplasty):
(Click here to read more about corneal transplantation.)
- Phakic Intraocular Lenses (IOLs):
- Purpose: To improve vision in cases where contact lenses or glasses are not effective.
- Procedure: Implantation of a lens inside the eye without removing the natural lens.
- Phakic Intraocular Lenses (IOLs):