Amblyopia
Amblyopia, often termed “lazy eye,” is a neurodevelopmental visual disorder where reduced vision in one or both eyes occurs due to abnormal visual development during early childhood. Unlike other visual impairments, amblyopia is not caused by structural defects within the eye itself but rather by the brain’s failure to process input from one eye properly. It is the leading cause of unilateral visual impairment in children, with a prevalence of approximately 2-3% worldwide. Amblyopia’s significance lies not only in its prevalence but also in its potential to cause permanent visual disability if not detected and treated early. This paper provides a comprehensive review of amblyopia, covering its pathophysiology, clinical presentation, diagnosis, management, and recent advancements in treatment.

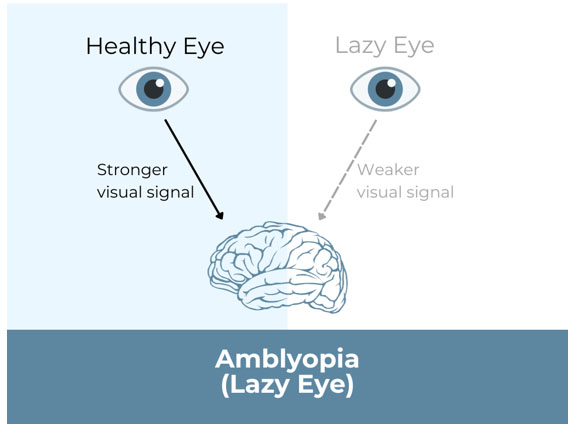
Amblyopia develops during the critical period of visual development, which extends from birth to around 7-8 years of age. During this time, the visual cortex is highly plastic, meaning that it is particularly sensitive to visual input. Any disruption in the quality or quantity of this input can result in abnormal visual processing and, consequently, amblyopia. The pathophysiology of amblyopia can be understood in the context of its three main types: strabismic, refractive, and deprivation.
Strabismic Amblyopia
Strabismic amblyopia arises from ocular misalignment, or strabismus, where the eyes are not properly aligned with each other. This misalignment causes the brain to receive different images from each eye. To avoid the confusion and diplopia (double vision) that would result from trying to merge these disparate images, the brain suppresses the visual input from the deviating eye. Over time, this suppression leads to amblyopia in the affected eye.
The development of strabismic amblyopia is highly dependent on the age of onset and the severity of the strabismus. If strabismus occurs early in life, particularly during the first few years, the risk of amblyopia is higher due to the brain’s heightened plasticity. The longer the misalignment persists without correction, the greater the risk of permanent vision loss.
Refractive Amblyopia
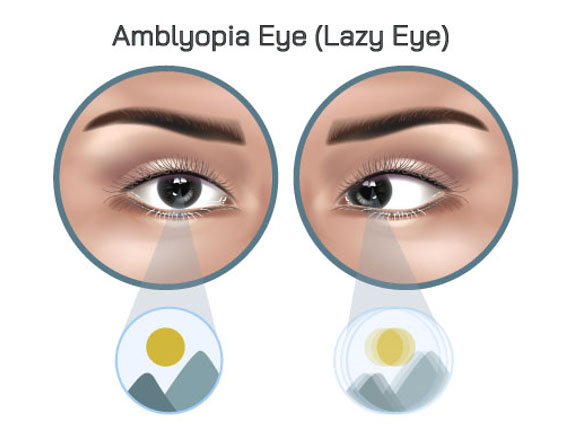
Refractive amblyopia occurs when there is a significant difference in refractive error between the two eyes (anisometropia) or when both eyes have high refractive errors (isoametropia). In anisometropia, the brain receives a clearer image from one eye and a blurred image from the other. To avoid processing the blurred image, the brain suppresses input from the eye with the higher refractive error, leading to amblyopia.
Isoametropic amblyopia occurs when both eyes have high refractive errors, such as hyperopia (farsightedness), myopia (nearsightedness), or astigmatism. In this case, both eyes receive equally poor images, which can lead to bilateral amblyopia if the condition is not corrected early. However, amblyopia from isoametropia is generally less severe than that from anisometropia, as the visual input from both eyes is more similar.
Deprivation Amblyopia
Deprivation amblyopia is the most severe form of amblyopia and occurs when visual input to one or both eyes is obstructed. This obstruction can result from conditions such as congenital cataracts, ptosis (drooping of the upper eyelid), corneal opacities, or severe ptosis. The lack of visual stimulation during the critical period of development results in poor visual cortical development and profound amblyopia.
Deprivation amblyopia can develop rapidly and lead to severe visual impairment if not treated promptly. Unlike other forms of amblyopia, which may have a more gradual onset, deprivation amblyopia can cause significant vision loss within weeks to months, making early detection and intervention crucial.
The clinical presentation of amblyopia varies depending on the underlying cause and the severity of the condition. In many cases, amblyopia is asymptomatic, particularly in young children who may not be aware of the visual impairment or unable to articulate it. However, there are several signs and symptoms that can alert clinicians and parents to the possibility of amblyopia.
Signs and Symptoms
- Reduced Visual Acuity: The hallmark of amblyopia is a reduction in visual acuity in one eye (or both eyes in bilateral cases) that cannot be corrected with glasses or contact lenses. This decrease in vision is typically detected during routine vision screenings or eye exams.
- Strabismus: Children with strabismic amblyopia may present with visible eye misalignment, where one eye turns inwards (esotropia), outwards (exotropia), upwards (hypertropia), or downwards (hypotropia). Strabismus is often the first sign of amblyopia that parents or caregivers notice.
- Difficulty with Depth Perception: Amblyopia, particularly in unilateral cases, can impair depth perception and binocular vision. This may manifest as difficulty judging distances, bumping into objects, or poor hand-eye coordination.
- Squinting or Head Tilting: Children with amblyopia may squint or tilt their heads to use their better-seeing eye, particularly when trying to focus on detailed tasks such as reading or drawing.
- Poor Academic Performance: Uncorrected amblyopia can affect a child’s performance in school, particularly in activities that require good vision, such as reading and writing. Teachers may notice that the child struggles with visual tasks or seems uninterested in activities requiring close attention to detail.
Diagnosing amblyopia requires a thorough eye examination to assess visual acuity, ocular alignment, refractive error, and the overall health of the eyes. Early detection is critical, as the success of treatment decreases with age. The following diagnostic tools and techniques are commonly used to identify amblyopia:
Visual Acuity Testing
Visual acuity is assessed using age-appropriate charts, such as the Snellen chart for older children and adults, or picture and letter charts for younger children. Each eye is tested separately to detect any discrepancy in visual acuity. In infants and non-verbal children, preferential looking tests or visual evoked potential (VEP) testing may be used to assess visual function.
Refraction
Cycloplegic refraction is performed to accurately measure refractive errors by temporarily paralyzing the ciliary muscle, preventing the eye from changing its focus during the exam. This is particularly important in detecting anisometropia or isoametropia, which may be contributing to amblyopia.
Ocular Alignment Assessment
Tests such as the cover-uncover test, alternate cover test, and Hirschberg test are used to assess ocular alignment and detect strabismus. These tests help determine if one eye is deviating from the visual axis and whether the brain is suppressing its input.
Fundus Examination
Ophthalmoscopy is performed to examine the retina, optic nerve, and other internal structures of the eye. This examination helps rule out any structural abnormalities, such as retinal detachment or optic nerve hypoplasia, that could explain the reduced vision.
Amblyopia Detection Tools
In addition to standard eye exams, specific tools like the Amblyopia Treatment Study HOTV visual acuity protocol or the Lea Symbols chart can be used to diagnose amblyopia in children. These tools are designed to engage young children in a way that makes it easier to assess their vision accurately.
The primary goal of amblyopia treatment is to improve visual acuity in the affected eye(s) and restore normal binocular vision. Treatment is most effective when initiated during the critical period of visual development, but older children and even adults may still benefit from intervention.
Corrective Lenses
Corrective lenses (glasses or contact lenses) are prescribed to correct refractive errors and provide clear visual input to both eyes. In cases of refractive amblyopia, correcting the refractive error alone may lead to significant improvement in vision. However, additional treatment is often required to fully resolve the amblyopia.
Occlusion Therapy (Patching)
Occlusion therapy is the most common treatment for amblyopia, particularly in cases where one eye is significantly weaker than the other. Patching involves covering the stronger eye with an adhesive patch for several hours each day, forcing the brain to use the amblyopic eye. The duration and frequency of patching depend on the severity of amblyopia, the child’s age, and how well the child tolerates the treatment.
Studies have shown that patching is highly effective, particularly in younger children, and can lead to significant improvements in visual acuity. However, compliance can be a challenge, as some children may resist wearing the patch. Educating parents about the importance of consistent patching and providing support to encourage compliance are crucial components of successful treatment.
Atropine Therapy
Atropine drops are an alternative to patching for treating amblyopia. Atropine works by temporarily blurring vision in the stronger eye, encouraging the use of the amblyopic eye. This method is often preferred for children who are non-compliant with patching, as it is less invasive and easier to administer.
Atropine therapy has been shown to be as effective as patching in many cases, particularly for moderate amblyopia. However, it may not be suitable for all children, especially those with light-colored eyes, as the drops can cause prolonged dilation and light sensitivity.
Vision Therapy
Vision therapy, also known as orthoptics, involves structured visual exercises designed to improve binocular vision and enhance the visual function of the amblyopic eye. These exercises may include activities to improve eye tracking, focusing, and coordination between the two eyes. Vision therapy is often used in conjunction with other treatments, such as patching or atropine, and can be particularly beneficial for children with strabismic amblyopia.
While vision therapy can be effective, it requires a significant time commitment from both the child and the parents, and the results can vary depending on the severity of the amblyopia and the child’s age.
Surgical Intervention
In cases of strabismic amblyopia where the misalignment of the eyes cannot be corrected with glasses alone, surgical intervention may be necessary to align the eyes. Strabismus surgery involves tightening or loosening the eye muscles to correct the deviation. While surgery can improve the cosmetic appearance of the eyes and enhance binocular vision, it is not a standalone treatment for amblyopia. Post-surgical therapy, such as patching or atropine, is typically required to fully rehabilitate the amblyopic eye.
For cases of deprivation amblyopia caused by congenital cataracts, early surgical removal of the cataract is crucial to prevent severe visual impairment. The timing of surgery is critical, as the longer the visual pathway is deprived of normal input, the greater the risk of irreversible amblyopia.
The prognosis for amblyopia varies depending on several factors, including the type and severity of amblyopia, the age at which treatment is initiated, and the child’s compliance with therapy. Early detection and intervention are key to achieving the best outcomes, as the plasticity of the visual system decreases with age.
- Strabismic Amblyopia: Children with strabismic amblyopia who receive early and consistent treatment often achieve good visual outcomes. However, if strabismus persists or recurs after treatment, there is a risk of amblyopia returning.
- Refractive Amblyopia: The prognosis for refractive amblyopia is generally good, particularly if the refractive error is corrected early. Many children with refractive amblyopia achieve normal or near-normal vision with appropriate treatment.
- Deprivation Amblyopia: The prognosis for deprivation amblyopia depends on the cause and timing of treatment. Early surgical intervention for conditions like congenital cataracts can significantly improve outcomes, but delayed treatment may result in permanent vision loss.
Long-term follow-up is essential for all children with amblyopia, as the condition can recur even after successful treatment. Regular eye exams and continued use of corrective lenses, if necessary, help ensure that the gains made during treatment are maintained.
In recent years, there have been several advances in the treatment of amblyopia that offer new hope for patients, particularly those who do not respond well to traditional therapies.
Binocular Approaches
Traditional amblyopia treatment focuses on monocular therapy, such as patching or atropine, which isolates the amblyopic eye. However, recent research has explored the potential of binocular approaches that involve both eyes working together. These approaches aim to improve binocular vision and reduce suppression of the amblyopic eye, leading to more integrated visual processing.
One promising method is the use of dichoptic training, where patients view images through special glasses that present different visual information to each eye. The brain is encouraged to combine the images, promoting binocular integration and improving vision in the amblyopic eye.
Video Game Therapy
Video game therapy is an innovative approach that has gained attention for its potential to treat amblyopia. Specially designed video games require the amblyopic eye to participate actively, encouraging visual processing and improving visual acuity. Studies have shown that playing these games can be as effective as traditional patching in some cases, with the added benefit of being more engaging for children.
Pharmacological Approaches
In addition to atropine, other pharmacological treatments are being investigated for their potential to enhance the efficacy of amblyopia therapy. For example, levodopa, a dopamine precursor, has been studied for its ability to improve visual outcomes when used in conjunction with traditional therapies. The results have been mixed, but ongoing research continues to explore the potential of pharmacological agents to boost the effectiveness of amblyopia treatment.
Amblyopia is a common but serious condition that requires early detection and prompt intervention to prevent permanent visual impairment. Understanding the pathophysiology, clinical presentation, and treatment options for amblyopia is essential for healthcare providers to effectively manage the condition and improve outcomes for affected children. Advances in treatment, including binocular approaches and video game therapy, offer new hope for patients who do not respond to traditional therapies. As research continues to evolve, the future of amblyopia treatment looks promising, with the potential for more effective and personalized interventions that address the unique needs of each patient.
Reference list
Amblyopia Treatment – AccuVision Eye Clinic. (n.d.). AccuVision – the Eye Clinic. https://www.accuvision.co.uk/amblyopia-treatment/
Boyd, K. (2020, March 4). Amblyopia: What Is Lazy Eye? American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/amblyopia-lazy-eye
Dr. Jennifer Ash. (2024, April 7). Amblyopia (Lazy Eye) – Symptoms, Causes and Treatment. Eye-Deology Vision Care; Eye-deology Vision Care. https://www.eye-deology.com/fyeyes/amblyopia-lazy-eye-symptoms-causes-treatments
eo.